A community perspectives piece by Ronna Wertman
As the world adjusts to living with COVID-19, millions of people remain missing from their everyday lives due to a chronic illness that many are not aware of. The medical community often provides incorrect advice and lacks proper institutional funding to find treatments and a cure.
This disease is myalgic encephalomyelitis (ME), also known as chronic fatigue syndrome (CFS). Each year on May 12, #MEAction recognizes the millions globally impacted by ME/CFS.
ME/CFS is a multi-system disease that causes profound metabolic dysfunction and is accompanied by physical and cognitive limitations. People experience symptoms on a spectrum from severe to mild and develop most notably post-exertional malaise (PEM), a worsening of symptoms after physical, emotional, or cognitive exertion. In most cases, ME/CFS is initiated by an infection.
Many people with ME/CFS anticipated the increase in post-viral illnesses because it happened with previous viral epidemics. They raised the public health alarm, yet our governmental institutions failed to adequately prepare for the wave of people with new or worsened chronic illnesses due to COVID-19. It is leading to a mass-disabling event.
Preliminary studies now show nearly half of people with Long COVID are presenting with ME/CFS.
Virginia U.S. Senator Tim Kaine continues to have unexplained chronic nerve tingling two years after a mild case of COVID. In March 2022, Sen. Kaine led the introduction of the Comprehensive Access to Resources and Education (CARE) for Long COVID Act to help address gaps and expand resources for those struggling with Long COVID and related post-viral illnesses.
The pathway to recovery or diagnosis for people with Long COVID will not be uniform. Some will recover, some will not, and others will develop a range of chronic illnesses like ME/CFS, autonomic disorders, and autoimmune conditions.
In particular, ME/CFS has long been an under-funded, under-researched, and feminized illness despite impacting people regardless of age, race, ethnicity, or gender. It affects more than one million Americans, with a total estimated 15 to 30 million people worldwide, and has a disease burden higher than that of MS or HIV/AIDS.
I have been navigating my own set of complex, chronic symptoms. When I began seeking skilled care, a local infectious disease specialist openly told me during my 40-minute consult, “I don’t believe in Long COVID.” A few months later, my primary care office’s nurse listened for ten minutes straight as I listed off my new symptoms during my follow-up appointment.
I appreciated her empathy. She noted how many patients come in now with similar accounts and the disbelief and dismissal she also experienced during her health care.
We are at a tipping point to change the narrative. The more we discover about the causes and symptoms of ME/CFS, Long COVID, and other under-resourced complex, chronic illnesses, the closer we move toward finding their connections and, potentially, treatments and a cure.
We must keep up the pressure and call on our leaders and institutions to undo decades of neglect and inaction that have systematically left millions of patients without recognition, treatment, or support.
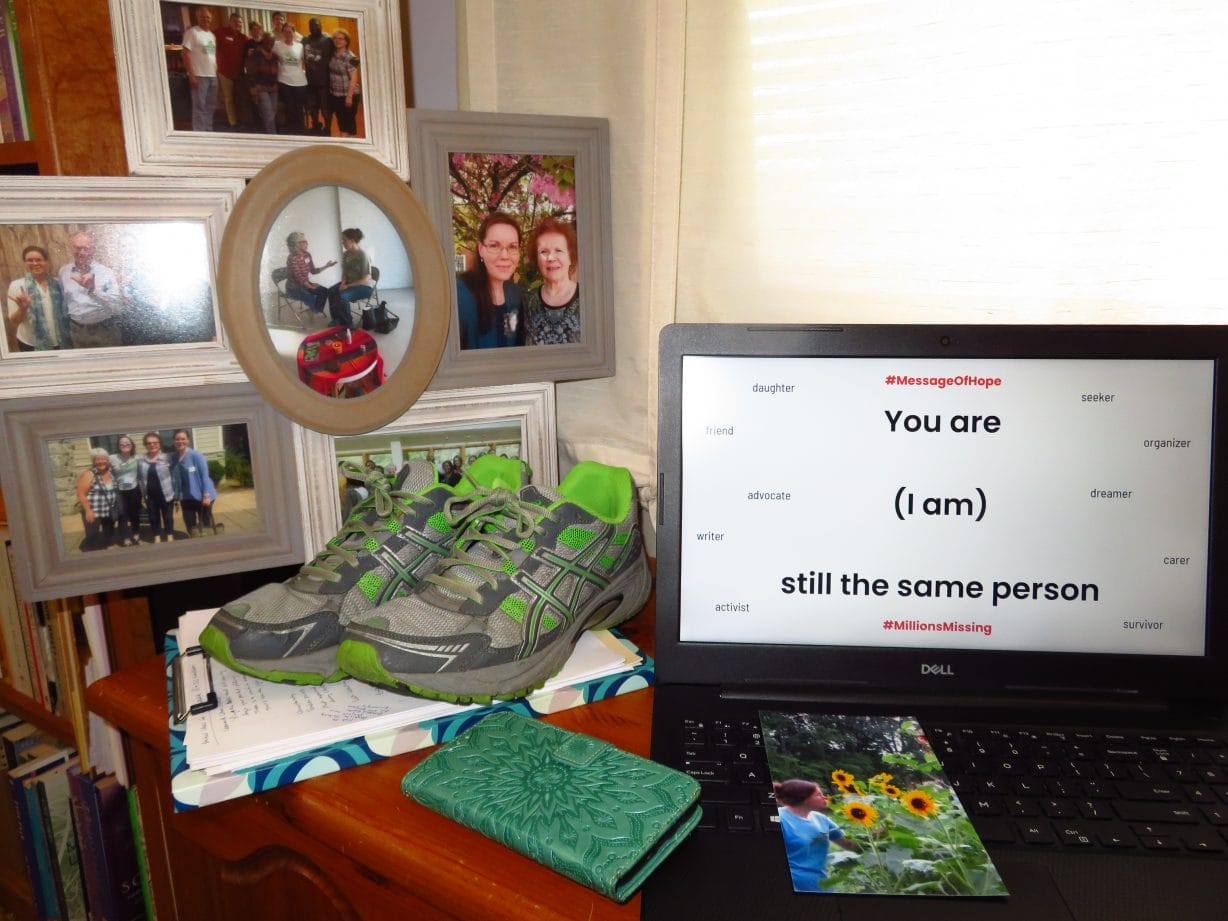
I am grateful to find the work of the non-profit #MEAction and countless other patient advocates, new and old, joined in this fight. They are here year-round to let you know you are not alone.
You do not have to fight alone. To learn more and get involved for yourself or someone you know and support, visit meaction.net. The more we connect and lift up the #MillionsMissing, the closer we are to change.
Ronna Wertman is a lifelong resident of the Shenandoah Valley and an advocate for many issues, with a focus on disability, language, and healing justice and health care access for marginalized communities. She is also a volunteer leader with Virginia Organizing, a statewide nonprofit nonpartisan community organization.












